IMMOBILIZATION DEVICE FOR PATIENTS UNDERGOING RADIATION THERAPY FOR HODGKIN’S DISEASE
By Gunilla C. Bentel, RN, RTT
Duke University Medical Center
Durham, North Carolina
INTRODUCTION
Hodgkin’s disease is a quite curable disease which strikes approximately 7400 young Americans annually, the majority of them less than 35 years old. This disease, which earlier was considered fatal, is now always considered curable in previously untreated patients. Great progress has been made in multi-disciplinary management of Hodgkin’s disease can be attributed to improved radiation therapy techniques. The ability to customize the shape of the treatment fields, the ability to treat contiguous lymphatic sites in a single field, and the capability to treat these large opposed fields without having to change the patient’s position represent some very important improvements. Improved diagnostic technologies also play an important role in the determination of the spread of the disease and, thus, aid in the choice of treatment strategy.
Appropriate treatment decisions in the management of cancer is always important for successful outcome but, in the management of Hodgkin’s disease, it is especially critical. The radiation dose prescription for Hodgkin’s disease presents a dilemma in which a balance must be struck between two conflicting end points: the use of doses high enough to eradicate the tumor and low enough to cause little or no injury to normal tissue. Serious attention must therefore be given to precision in the delivery of the often complex radiation therapy treatment in these relatively young and curable patients.
Marks and Haus has presented data with respect to misalignment of treatment fields in patients with Hodgkin’s disease and non-Hodgkin’s lymphoma.5,9,10 They found, in a retrospective review of port films of 902 set ups on 99 patients with Hodgkin’s disease and other lymphomas, that 36% of the treatment fields were erroneously placed. In 10 of 99 patients disease was not controlled locally. Two of these failures were at the margins of the fields and were shown by portal films to be correlated with positioning errors leading to reduced dose at the sites of recurrence. One might conclude that errors in treatment delivery including immobilization errors, may be a significant cause of marginal recurrences.
Taylor et al. found 15% of mantle fields in error by more than 5 mm in 28 patients (1186 films).14 There was no tumor or prophylactic treatment area shielded in these misaligned fields. Only 1% of the fields studied was considered unacceptable. The anterior field was treated with the patient supine and immobilized using a bite block and face mask system while the posterior field was treated with the patient prone and positioned in an ALPHA CRADLE® form.
Hulshof et al. studied 216 set ups of mantle fields and found that on the first port film, at the start of the treatment, 13% of the set ups were in error by more than 10 mm.6 Following the first correction, an adequate treatment set up was obtained in 60% of cases and after the second correction the adequacy rate was 84%. Creutzberg et al. compared 94 megavoltage portal films with 26 simulation films and found that alignment errors in excess of 10 mm occurrence in 7.2% of cases.2 Other authors have attributed small errors observed on the initial portal field to discrepancies between alignment systems in the simulator room and the treatment room.3,4,7,11,12,13 Both Hulshof and Creutzberg reported a larger error rate observed on posterior fields treated with the patient in the prone position. Maintaining the patient’s position supine for all fields improves not only the reproducibility but it also improves the dose uniformity across the junction of adjacent fields.
Kinzie et al.8 in a Patterns of Care study, reviewed port films of patients treated with radiation therapy alone. They found that inadequate margins were associated with a 54% overall relapse rate, of which 33% were in field or marginal recurrences. When the port films were judged to be adequate, the overall relapse rate was 14% with only 7% being in-field or marginal recurrences.
Reproducing the treatment fields precisely on a daily basis in order to avoid “geographic misses” and to minimize the volume of normal tissue being irradiated is crucial. Aggressive immobilization should be utilized to offer these patients the best possible chances for cure. Failure to controls the disease on the first attempt often constitutes a life-threatening situation for the patient. Judicious implementation of the initial treatment is therefore crucial. Further radiation therapy which may be necessary to treat recurrent disease is limited by the tolerance of the adjacent normal tissue and will increase the risks of long-term adverse consequences.
TREATMENT
The extent of radiation therapy in Hodgkin’s disease depends on the stage of the disease but it involves almost always total lymphoid irradiation (TLI) or subtotal lymph nodal irradiation. The lymph nodal groups above the diaphragm are the cervical, supraclavicular, infraclavicular, axillary, mediastinal, and hilar nodes. These are usually treated through large opposed anterior and posterior fields referred to as mantle fields.
In adult patients, the mantle field is often very large. The margins extend cephalad to include the submanibular nodes, caudal to the level of the diaphragm and lateral to include the axillary nodes. The field is shaped by customized shielding blocks which protect the lung parenchyma, the humeral head, and the distal part of the humerus bilaterally. Additional shielding blocks are added at appropriate dose levels to protect the left ventricle of the heart, the larynx and the cervical spinal cord.
The lymph nodal groups below the diaphragm are the para-aortic, pelvic, and inguinal lymph nodes. The splenic pedicle (or spleen, if it is in-situ) is also usually treated depending on the findings during a staging laparotomy. These lymph nodes are also usually treated through parallel opposed anterior and posterior fields. Depending on the stage of the disease, the pelvic and infuinal lymph nodes may not need to be treated. Fields designed to include the nodal areas below the diaphragm includes a very large volume of bone marrow, which, if treated concurrently, often causes hematopoietic depression. The para-aortic lymph nodes and the splenic pedicle are therefore often treated first and the pelvic and inguinal nodes are treated following a recovery period. These fields are also custom designed, using shielding blocks to protect as much as possible of bone marrow, liver, kidneys, bowel, and bladder.
The customized shielding blocks used in the treatment of the mantle and para-aortic-splenic fields are fixed to a tray which fits tightly into the collimator of the therapy machine. When the tray holding the blocks is inserted correctly in the beam, the treatment field is projected precisely as it was outlined on the radiograph from which it was formed. The only variables in the treatment geometry is the orientation of the treatment machine and the couch and in the patient’s position. The machine and couch variables can easily be eliminated by setting the prescribed angles while the variation in the patient’s position is more difficult to master. The large perimeter of the mantle and para-aortic/pelvic fields are very sensitive to small errors in misalignment between the radiation beam and the patient’s anatomy. An alignment error, which can occur even if the central axis of the beam is correct, becomes more severe as the distance from the central axis increases as shown in Fig. 1. Therefore, since the treatment fields used in the treatment of Hodgkin’s disease often are large, the patient-beam alignment is very important when these fields are treated.
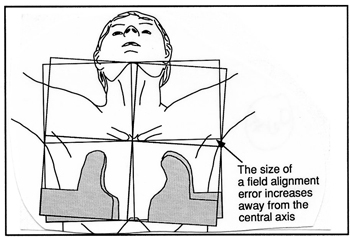
Fig. 1 A treatment field can be misaligned even when the central axis is set up correctly. The effect of a misaligned field increases as the distance from the central axis increases.
As described above, the lymph nodal areas are often treated sequentially in two or three adjacent areas through opposed fields leading to difficulties in matching field borders without causing overdosage at the field junctions. The use of the immobilization device described here reduces misalignment errors and also reduces the risks of inadvertent mismatch of the adjacent field margins.
POSITIONING DEVICE
The Patient’s Position
The patient’s position is supine with the arms raised above the head and the chin extended. This position is maintained during the treatment of all fields to minimize changes in the relationship between skin marks and the spinal cord near the field junctions. The extension of the chin allows the submental, submandibular, and cervical lymph nodes to be treated while keeping the oral cavity out of the treatment field. The arms are elevated in an effort to move the axillary lymph nodes out and away from the lung parenchyma. This allows shielding of the lung tissue while the margins around the axillary lymph nodes are increased.
An uncomfortable position is quite difficult to maintain for long periods of time. Therefore, it is fundamental to successful immobilization that the patient is provided with supports that will make the position comfortable. Such a device should also aid in reproducing the position from day-to-day. ALPHA CRADLE® forms (HS2) for positioning patients receiving radiation therapy for Hodgkin’s disease has been used in our clinic for approximately 15 years. The HS2 ALPHA CRADLE® form consists of a Styrofoam®* form which provides indentations for the elevated arms (45°) and offers a barrier for the foam around the patient’s head and thorax. The foam, when prepared and used as directed by Smithers Medical Products, Inc., fills the space between the Styrofoam® and the patient’s skin and forms a perfect mold in which the patient can be repositioned for each treatment. This ALPHA CRADLE® form, which only reaches to the patient’s waist and offers no comfortable place for the patient to rest the hands, was used in our clinic for approximately 10 years. The difficulties with field alignment were reduced, particularly when the mantle fields were treated, but not to our satisfaction. Since this ALPHA CRADLE® form offered no reliable method by which to reproduce the arm elevation, a handle which the patients hold onto during the treatments, was added.1 Reproducing the arm elevation precisely each day reduces the risk of the skin marks moving and overlay different internal anatomy. An improvement in set up reproducibility of the mantle fields was observed, while the difficulties with reproducing the para-aortic/pelvic fields continued. More recently, another modification, described in this report, has been made to the HS2 ALPHA CRADLE® form.
*Registered by Dow Chemical
Fabrication of the immobilization device
The set up difficulties which we continued to experience was thought to be the result of only the chest being aligned with the sagittal alignment line when the mantle field was treated, or the abdomen when the para-aortic nodes were treated. The immobilization device was therefore extended caudally to also immobilize the pelvis and the thighs and so that the sagittal alignment line could be marked on the immobilization device at two points separated by a long distance (Fig 2).
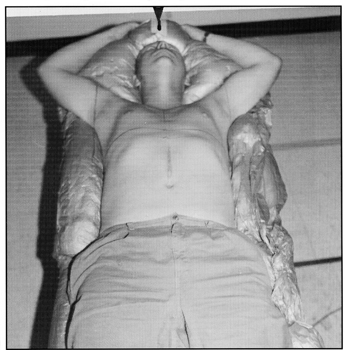
Fig. 2 The HS2ME, extended Alpha Cradle® form extends to the knees in most adult patients making it possible to make alignment marks (arrows) both above the head and between the knees.
The standard ALPHA CRADLE® form with the grooves for arm elevation at 45° is modified to include a base which is 5’ long, becoming the HS2ME. This base extends to just below the knees in most adult patients. Several pieces of Styrofoam® are cut and added to the base at points which are determined with the patient in the form but without the foam. A rectangle of Styrofoam® approximately 2” wide, 4” long, and 1” high, is placed in the center of the ALPHA CRADLE® base between the patient’s knees (Fig. 3A). The foam will raise up between the knees and form an elevation which is used for marking the sagittal alignment line (Fig. 3B).
The second sagittal alignment mark is made on the Styrofoam® form above the patient’s head. These two alignment marks are used in the daily repositioning of the patient on the couch. A small triangular-shaped Styrofoam® block is placed under each knee to relax the patient’s back. Two Styrofoam® cylinders, approximately 3” long and 1” in diameter and formed from the Styrofoam® used for customized block cutting, are placed in a separate bag which is positioned where the patient’s raised arms and hands will be positioned. A retaining wall of Styrofoam® is added to each side of the base to help force the foam in toward the patient’s torso.
With the patient removed, each piece of Styrofoam® is taped to the base and the entire ALPHA CRADLE® form is placed inside a large protective polyvinyl bag. Before the patient is returned to the mold, one set of foam (660 cc)* is prepared as directed by the manufacturer. Approximately 100 cc is poured inside the arm support bag holding the Styrofoam® cylinders and the remainder is evenly distributed inside the form. Several small holes are made in the arm support bag on the side which is toward the Styrofoam® form to allow some foam to leak and form a glue which attaches the small bag to the rest of the mold. Alternatively, a small amount of foam can be poured on top of the Styrofoam® form under the smaller bag. If the bag with the handles is not attached to the HS2, it can move causing problems with repositioning of the arms.
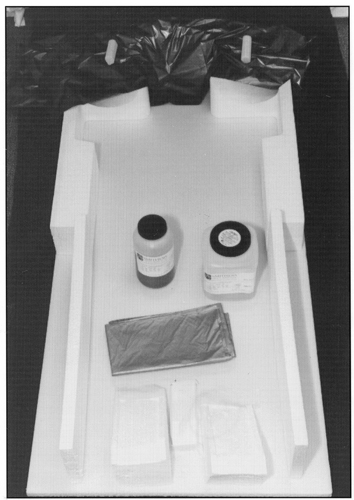
Fig. 3A Several pieces of Styrofoam are added to the HS2ME, extended Alpha Cradle® form. The dark bag seen near the head segment of the Styrofoam form is for the arm support and handles. The entire form and the dark bag are placed inside the larger bag before the foam is poured.
*In some patients it may be necessary to use an additional 250 or 375 cc of foaming agents.
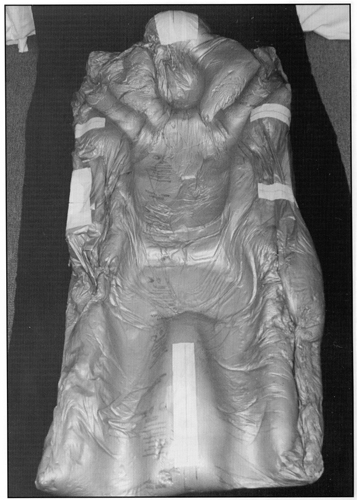
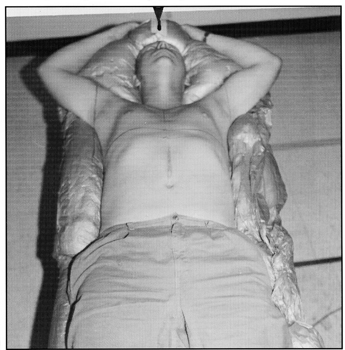
Fig. 3B The finished extended Alpha Cradle® form creates a comfortable, tight fitting mold for the patient.
After approximately 60 seconds, during which time air is allowed to circulate inside the bag, the air is squeezed out, the bag is sealed, and the patient is returned to the form. The patients enter the form body first sitting on the couch near the caudal edge of the ALPHA CRADLE® form and then gradually lift and move the buttocks over the knee supports and into the form. A visual check is made to see that the patient appears straight on the mold and they seed that the patient appears straight on the mold and they are asked to adjust the chest and hips until they feel straight. The patient’s arms are elevated to desired position and the Styrofoam® handles are moved into the patient’s hands. The foam is pushed up around the hands and the arms. Masking tape is fastened to the sides of the ALPHA CRADLE® and is stretched across the patient’s body to force the two sides in toward the patient to form a tight-fitting mold. Foam is also forced up between the patient’s knees where the sagittal alignment line is later marked. A chinstrap, made of Velcro®**, is used to aid the patient in maintaining the chin extension.
**Registered by Velcro USA
A board, which is wider and longer than the extended ALPHA CRADLE® form, is placed on top of the couch before the ALPHA CRADLE® form fabrication is initiated to prevent leaking foam from forming a lip over the couch. Such lip or other irregular surface under the ALPHA CRADLE® form and consequently of the patient giving rise to field misalignments.
The foam stops expanding after approximately 7-10 minutes but requires an additional 10 minutes to become firm. During this time, the patient is asked to think about how it feels to lay in the mold so that when they are repositioned, they can adjust their body until it feels the same.
To produce a tight-fitting mold, it is important that the patient wears minimal clothing during the extended ALPHA CRADLE® form fabrication. Since patients usually wear different clothing each day during the course of treatment, the mold may be too large some days and too tight on other days. Both situations would compromise the ability to correctly reposition the patient.
PATIENT-BEAM ALIGNMENT
Prior to the simulation procedure it is crucial that the machine settings, i.e., the couch, collimator, and gantry angles are all sat to 0°. The sagittal alignment line is marked in the patient’s midline which is found either by palpation of the sternum and pubis symphysis or by viewing the spinal column in fluoroscopy. The sagittal alignment line is also marked on the elevation of the ALPHA CRADLE® form between the patient’s knees and on the positioning device above the patient’s head. If the polyvinyl bag is not fixed to the mold, it is best to peel it away and make the marks directly on the foam eliminating any chance that the mark may move. Since many alignment systems are less reliable farther from the isocenter, it is necessary to move the couch so that each of the two marks are made near the isocenter, i.e., move the couch out from the gantry to make the mark above the head and move in toward the gantry to make the mark between the knees.
The treatment fields are then simulated in the usual fashion and the fields are marked on the patient’s skin surface. The transverse sand lateral (horizontal) alignment lines are marked on the ALPHA CRADLE® form to aid in the treatment set up in the even that the marks on the skin are worn off or migrate during re-marking each day. By aligning the four alignment lines with the marks made on the ALPHA CRADLE® form, the position can be reproduced for each treatment without marks on the patient’s skin. The caudal extent of the mantle field is tattooed on the patient’s skin on the anterior chest to aid in setting the gap between the mantle and the para-aortic fields when the patient returns 2 to 3 weeks later.
When the patient returns for the para-aortic/pelvic treatment, the position is resumed in the same ALPHA CRADLE® form. A gap is calculated between the mantle and the para-aortic fields. During the simulation of the para-aortic field, a lead marker is placed on the tattoo indicating the caudal margin of the mantle field. If the gap is sat correctly, the cephalad margin of the posterior para-aortic field should traverse the spinal column at the same level as the caudal margin of the anterior mantle field (Fig. 4). The para-aortic field is also tattooed on the patient’s abdomen and in the case of subsequent pelvic/inguinal node irradiation, the gap is similarly determined and marked.
All treatment fields are defined by customized blocks and are treated using a linear accelerator*. Mantle fields are treated using a 6 MV photon beam while in some patients the para-aortic fields are treated using 15 MV photons. The patients are invariably treated in the supine position, i.e., the posterior beam traverses the extended ALPHA CRADLE® form. No adverse skin reaction has been noted and no correction for attenuation by the foam material has been made. All fields area treated using an isocentric technique except if an extended distance is required in order to include the entire treatment area in a single field.
*Siemens Medical Systems, Inc
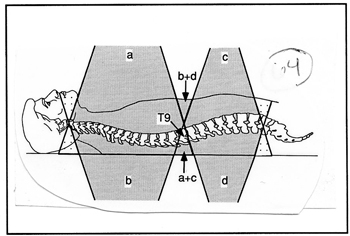
Fig. 4 A gap between the mantle and para-aortic fields calculated so that all beam edges converge at the mid-depth provide the most uniform dose distribution. Although it appears, when looking at the radiographs of the two anterior fields, as if the fields overlap in the spinal column, the dose there is low because this area lies in the exit of both beams and are outside both of the posterior fields. The segment of the spinal column “seen” in the anterior mantle field should be outside the posterior para-aortic field when the field gap is sat correctly.
PORT FILM REVIEW
The reproducibility of the patient-beam alignment is documented through weekly port films. On the first treatment day, port films are taken of both the anterior and the posterior fields. If no misalignment is noted, subsequent port films are taken of the anterior and posterior fields on alternate weeks. If a misalignment is noted, a correction is made on the following treatment and another port film is taken.
Small discrepancies between alignment systems in the simulator room and the treatment room and varying amount of sag in the two couches may cause small errors in patient alignment on the first set of port films3,4,7,11,12,13, however, in evaluating the effect of the extended ALPHA CRADLE® form described above, all port films were included. To assess the effect of the extended ALPHA CRADLE® form described in this report, only the monitoring physician’s routine review of port films was used. When a port film was taken of the anterior and the posterior fields on the same day, it was recorded as only one port film day since it represented only one set up.
PATIENT CHARACTERISTICS
To assess the effect of the extended ALPHA CRADLE® form, the number of misalignments observed on port films was compared with that of the same number of patients treated using an ALPHA CRADLE® form which had an arm support and handles but extended only to the waist. Ten patients with Hodgkin’s disease were treated between February and August 1993, using the HS2 ALPHA CRADLE® extended form. These 10 patients represented 53 mantle port film days and 22 para-aortic or para-aortic/pelvic film days. The earlier group of 10 patients were treated between April 1992 and January 1993 and represented 63 mantle port film days and 42 para-aortic or para-aortic/pelvic film days. In both groups, other fields were also treated (Waldeyer’s ring, mediastinal boost, inguinal nodes, etc.) however, these fields were not included in the analysis due to the inability of matching these fields in the two groups. It would not be a fair evaluation of the effect of the extended ALPHA CRADLE® forms if the patients with which to compare the set up accuracy had been selected such that the two groups would have the same treatment fields. The patients in the earlier group represented the 10 Hodgkin’s disease patients treated immediately prior to the implementation of the extended ALPHA CRADLE® form.
RESULTS
Review of the mantle port films revealed that the set up reproducibility was excellent in both groups with a 6.3% misalignment rate (4 in 63 set ups) in the group using the short ALPHA CRADLE® form and 5.7% (3 in 53 set ups) in the group using the extended HS2 ALPHA CRADLE® (HS2-M) form.
In the para-aortic or para-aortic/pelvic port films, there was a 42.9% misalignment rate (18 in 42 set ups) in the group using the short ALPHA CRADLE® form and 9.1% (2 in 22 set ups) in the group using the extended ALPHA CRADLE® form.
The overall misalignment rate was therefore 21% (22 in 105 set ups) in the group using the short ALPHA CRADLE® form and 6.7% (5 of 75 set ups) in the group using the extended ALPHA CRADLE® form. The size of the misalignment errors, as indicated by the monitoring physician, was larger in the group using the short ALPHA CRADLE® form with 5 being > 10 mm while in the group with the extended ALPHA CRADLE® form all shifts were < 5 mm.
It is interesting to note that two of the three set up errors in the mantle treatment and one in the para-aortic treatment in the group using the extended HS2 ALPHA CRADLE® form, occurred in the same patient. The patient was a young male who was non-compliant with the treatment schedule and came for treatment on an irregular basis. The only other set up misalignments in this group was a 5 mm shift in a mantle fields and a 3 mm shift in a para-aortic field.
In addition to finding these convincing numbers, the technologists feel that they can set up the treatment faster when the patients are positioned in a body mold. The reduced number of repeat port films also saves the technologists’ time, both in terms of taking and developing the films, and it also reduces the physicians’ time because there are less port films to review. Other savings are recognized in terms of amount of films needed and in space required for film storage. The most important gain, however, lies with the fact that the patients’ feel comfortable and relaxed with the handles and are secure on the narrow treatment couch.
DISCUSSION
Radiation therapy in the often young and curable patients with Hodgkin’s disease require careful planning and implementation. Long term adverse consequences of the treatments must be minimized by sparing as much as possible of adjacent normal tissue. Serious attention must therefore be given to the precision with which the treatments are delivered. Aggressive immobilization techniques may reduce set up errors and lead to improved survival. The ALPHA CRADLE® form, HS2-M Extended, described in this report represent one improvement which may have a role in the final outcome of the treatment for patients with Hodgkin’s disease.